Our History
From small beginnings to worldwide leaders
The ACPCC was originally founded as the Victorian Cytology Service (VCS) in December 1964 as a joint venture initiative between the Victorian State Government, the Cancer Council and Prince Henry’s Hospital. We were established to provide cervical cancer screening services to Victorian women following the introduction of the Pap smear. In 1965, we began operating from Prince Henry’s Hospital where we stayed until 1991.
In 1991, VCS was incorporated and moved from the hospital to Faraday Street in Carlton, Victoria. This was also the year that the National Cervical Screening Program was established as a joint initiative of Australian State and Territory Governments.
Over our 57-year history, ACPCC continued to expand its services. In 2012, we established VCS Pathology. This was followed by Digital Health in 2017 and Population Health in 2018.
Changing our name
On 8 November, 2021 we changed our name from VCS Foundation Ltd to the Australian Centre for the Prevention of Cervical Cancer. This name change ensures that we are recognised as Australia’s leading organisation in cervical cancer screening and prevention, which is an important step in our goal to eliminate cervical cancer as a public health problem in our region. On the same day, we also launched the Australian HPV Reference Laboratory.

Pioneering achievements
- In 1989, we established the first Pap Test Registry in Australia to support an organised approach to cervical cancer screening.
- 2008 saw us establishing and operating the world’s first HPV vaccination program register on behalf of the Australian Department of Health.
- We were a driving force in providing evidence to support the Australian Government’s decision to transition from 2 yearly Pap tests to 5 yearly HPV tests in the renewed National Cervical Screening Program, which commenced in December 2017.
- In 2018, we became the first laboratory in Australia to achieve accreditation for processing HPV self-collection tests after undertaking a rigorous in-house validation process. This is a key achievement, given that self-collection is the most important tool in Australia’s belt to achieve elimination of cervical cancer by 2035.
- 2021 brought our launch of the Australian HPV Reference Laboratory to enhance and monitor the performance of HPV tests, technology and laboratory procedures to help reduce HPV-related disease.
2018
Restructure of organisation to VCS Foundation
VCS Population Health introduced
2017
VCS Digital Health introduced
VCS ICT Platform canSCREEN upgraded for commercial market
Restructure of VCS workforce to support the renewed NCSP
12722025 smears reported from 1965 to the commencement of the renewed NCSP
Renewal of the National Cervical Screening Program launched in December 2017
2016
VCS Shortlisted in tender for the operation of the National Cancer Screening Register but ultimately unsuccessful
ICT platform canSCREEN developed to support the future growth of the Victorian Cervical Cancer Screening Register and National Human Papillomavirus Register
Compass Main Trial recruitment target of 36,300 unvaccinated women born on, or before June 30th 1980 reached in May.
Total workforce prior to Renewal = 181
2015
12,006,312 Pap smears reported over the life of the service
VCS Celebrates 50 years of service
Compass Main Trial tor recruit 121,000 women commences
VCS hosts PCC2015, the third such conference.2015
2014
VCS appointed operators of the South Australian Screening Register added the service
2013
Boys added to the HPV vaccination program. VCS takes on some functions of the Bowel Screen Program in Victoria. Planning commences for a renewed cervical screening program.
Compass Pilot Study commences
National Bowel Screen Cancer Registry Follow Program (PFUF) added to the service
2012
Establishment of VCS Pathology
VCS rebranding and logo refresh
2011
VCS hosts PCC2011, the second such conference.
First data released by VCS showing a decrease in high grade abnormalities after introduction of the HPV vaccination program.
2010
20th anniversary of VCCR.2010
2009
Preventing Cervical Cancer Conference (PCC) bringing togeher Australian and International experts
Renewal of National Cervical Screening Program announced.
2007
National HPV Vaccination Program implemented.
2006
NHMRC Guidelines for the Management of Asymptomatic Women with Screen Detected Abnormalities.
2005
Implementation of MediPath LIS for histopathology.2005
2004
Planning started for determining a suitable site for VCS once RWH moves.
2003
CIS now had a decision support tool offering the reporting scientist or pathologist the appropriate clinical recommendation.
2002
Due to another Victorian laboratory losing its NATA accreditation, test volumes increased markedly for a period.
2001
CIS project completed July 2000. Victorian BreastScreen Registry relocated to new premises on 26 July 2000.
2000
On 17 August 1999, the core functions of the new CIS commenced.
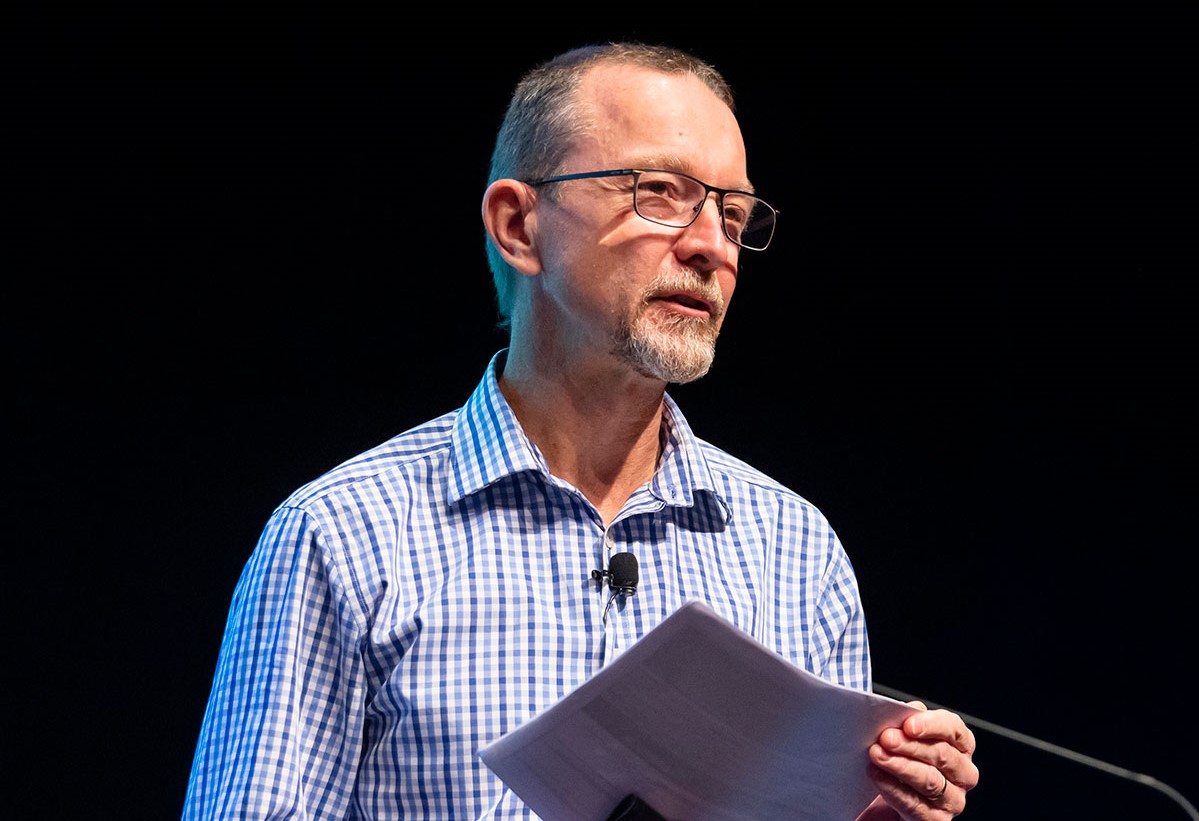
Dr Marion Saville appointed Director2000
1999
Mandatory for pathology laboratories to meet performance targets.
1998
VCS was providing a public cytology service for the Royal Melbourne Hospital.
1997
BreastScreen handled approximately 220,000 phone calls and made 158,000 appointments for women.
1996
Performance measures for Australian laboratories reporting cervical cytology introduced.
1995
VCCR and VBR required increased space.1995
1994
First NHMRC Guidelines Screening to Prevent Cervical Cancer: Guidelines for the Management of Women with Screen Detected Abnormalities.
1993
VCS commenced a contract to provide the Victorian BreastScreen Registry (VBR).
1992
Cancer Council Victoria and Victorian Cervical Cytology Registry introduced the "Organised Approach to Preventing Cancer of the Cervix"
1991
On 3 September 1991, VCS was incorporated.
National Cervical Screening Program established as joint initiative of Australian State and Territory Governments.
VCS moved from Prince Henry's to 265 Faraday Street Carlton
1990
The Commonwealth agreed to pay $1.5 million, matched by the State Government, to improve the Service in a number of areas.1990
1989
Bill passed. Amendment to Cancer Act 1958 Cancer (Central Registers) Act 1989. VCCR established under direction of Heather Mitchell - the first state-based Pap test Registry.
1988
Review of cervical screening in Australia commissioned. Working Party on Central Registry at ACCV and proposal to establish Registry. Extensive community consultation.
Dr Gabriel Medley Appointed Director
1987
Report of Anti Cancer Council of Victoria Working Party on Mass Screening for cervical cancer recommending formal statewide database.
1986
A survey by the Anti-Cancer Council showed that 20% of Victorian women had never had a cervical smear.
1985
May 1985 was a record month for smears, 29,442 were received.1985
1984
There were the first reports of occupationally related illnesses at the Service.
1983
Sir Lance Townsend, founding chairman died.
1982
On the 28th May 1982, the Minister for Health, The Honourable T. W. Roper visited the Service and personally supervised the registration of the three millionth smear.
1981
Despite a recommended two-yearly screening interval, Victorian women appeared to have set their own “mean interval” of 3.5 years.
1980
Univac V77/600 mini-computer replaced virtually all existing clerical activities1980
1979
In December 1979, VC(G)S celebrated 15 years.
Medical staffing continued to be a cause of concern since at no time since the inception of the Service had a stable medical staff structure been achieved.
1978
There was a reorganisation of medical staff with four Pathologists employed within the Department of Anatomical Pathology.
1977
RMIT established a degree course in applied science, which included Anatomical Pathology 1.
1976
Introduction of Medicare bulk billing allowed other laboratories to provide an apparently “free” service.
1975
The screened population coverage reached over 90% in some age groups.1975
1974
Staff efficiency was calculated to have doubled since the inception of the Service.
1973
The Clinical Cytology II subject commenced at RMIT.
1972
Average smear cost for the year was $1.16.
1971
137,717 smears were received, with 487 “positive” cases.
1970
Punch cards were used for ‘normal’ and ‘abnormal’ records, which were transferred onto magnetic tape.1970
1969
The Service moved into new premises on the third floor of the new clinical school at Prince Henry’s Hospital.
1968
Staff were divided into Cytotechnologists, Senior Cytotechnicians and Cytotechnicians (screeners).
1967
Screeners were mostly girls straight from matriculation.
1966
Over the first 18 months, 70,878 smears were examined, which was approximately 7% of the adult female population in Victoria.
Total workforce at the commencement of the service = 19.5
1965
Victorian Clinical Gynaecology Service established operating from Prince Henry's Hospital1965
1964
Victorian Cytology (Gynaecological) Service was formed on 9th December 1964.
Dr Michael Drake appointed Director
VISION
Our Vision
Et has minim elitr intellegat. Mea aeterno eleifend.Et has minim elitr intellegat. Mea aeterno eleifend.Et has minim elitr intellegat. Mea aeterno eleifend.Et has minim elitr intellegat. Mea aeterno eleifend.Et has minim elitr intellegat. Mea aeterno eleifend.
READ UP ON IT
Success Stories
Get in touch
To find out more about what we do or how we can work together, please get in touch.