Self-collection Saves Lives
Cervical Screening Campaign
Victorian campaign calls for health practitioners to increase cervical cancer screening through the self-collection option
The Australian Centre for the Prevention of Cervical Cancer (ACPCC) and Cancer Council Victoria are pleased to collaborate on a campaign to increase awareness of healthcare practitioners about HPV self-collection. HPV self-collection has recently been made available as a choice for all cervical screening participants in the National Cervical Screening Program.
Self-collection allows participants to take their own vaginal sample for HPV testing. It is an equally accurate and highly acceptable alternative to a healthcare practitioner-collected cervical screening test (CST) and is an important tool to increase cervical screening participation amongst under-screened and never screened groups, such as Aboriginal and Torres Strait Islander people, those living in regional and remote areas, people who are culturally and linguistically diverse, LGBTIQ+ communities and those living with disability.

Offering HPV self-collection in your practice will help more women and people with a cervix to be screened for cervical cancer, preventing devastating diagnoses and saving lives.
The Self-Collection Saves Lives campaign is aimed at health practitioners including GPs, nurses and antenatal health professionals.
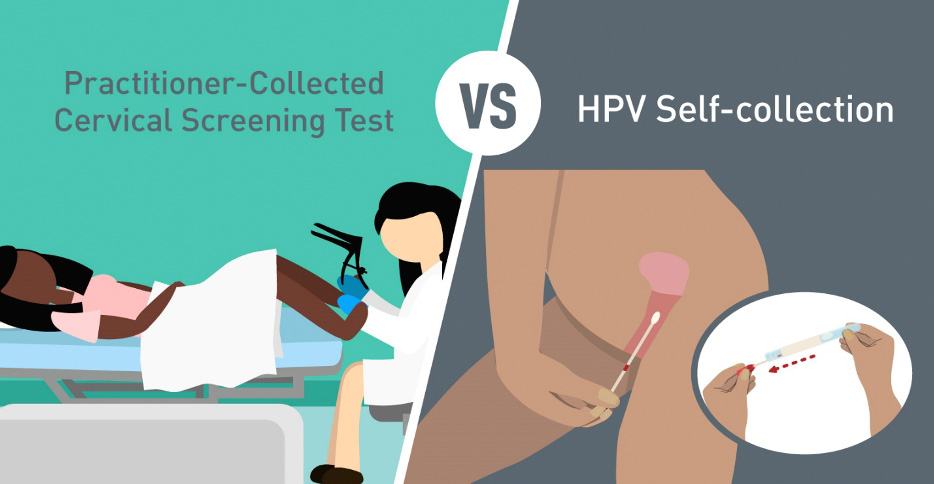
Figure 1: Cervical Screening Test vs HPV Self-collection
Image credit: Cancer Council Victoria (CCV)
WHO IS IT FOR
Who is eligible to take their own screening sample?
All people who are eligible for a cervical screening test can opt for self-collection: people aged 25-74, who are due or overdue for their routine cervical screening, who are not presenting symptoms that suggest cervical cancer, and who don’t have any other reason to require a co-test.
People who may be uncomfortable with a speculum examination often find self-collection a much more acceptable alternative. Reasons for this discomfort can include cultural beliefs, previous negative experiences or past trauma.
There will be many for whom self-collection makes all the difference between not being screened and being screened.
HOW YOU CAN HELP
Please help us spread the word amongst your networks.
You can help boost the reach of our campaign by:
- Sharing ACPCC and Cancer Council Victoria’s campaign materials and webpage with your contacts and followers.
- Sharing information about our campaign across your social media channels, and like and share our social media posts.
- Sharing information about our campaign through your e-newsletters.

Facts about self-collection
Self-collected samples are as sensitive as clinician-collected cervical specimens for the detection of CIN2+/AIS and HPV (Arbyn et al 2018, Saville et al 2020).
Self-collection overcomes barriers to a speculum examination. Studies in Australia and New Zealand show high levels of acceptability of self-collection amongst First Nations peoples and other underscreened groups (Creagh et al 2021, Butler et al 2020).
Self-collection can be done at home. Practitioners can offer self-collection during a telehealth consultation. At your request, VCS Pathology sends a kit to your patient with instructions and a reply-paid envelope. Results are sent to you. Find more info about home based self-collection here.
Self-collection is now widely available. From 1st July 2022, self-collection is available as a choice to all women & people with a cervix through the NCSP. Make sure you are equipped with the right information to offer this to your patients. Check out the ew guidelines, watch the short video, and read the FAQs for Healthcare Providers here.
Self-collection Myths Busted
Self-collection is not as sensitive as a clinician-collected speculum examination. FALSE. Self-collected samples are as accurate as clinician-collected cervical specimens for the detection of CIN2+ /AIS and HPV (Arbyn et al 2018, Saville et al, 2020).
There is no point offering self-collection as an option, as my patient won’t return for follow up if the test detects HPV. FALSE. Pilot studies have shown that the vast majority of participants do return for follow up after an HPV-positive self-collected sample, however they may need additional support and encouragement from you.
Self-collection is not clinically indicated for pregnant women. FALSE. Self-collection can be offered during pregnancy – check with your pathology laboratory to ensure they are accredited to process samples from pregnant women. Routine antenatal and postnatal care should include a review of the patient’s cervical screening history. A woman can be safely screened at any time during pregnancy provided that the correct sampling equipment is used; a vaginal HPV swab is suitable.
Self-collection is not as effective because I can’t visualise the cervix. FALSE. There is no evidence to support pelvic examination/visualisation of the cervix as routine practice for asymptomatic patients (ACOG 2018, RACGP). For HPV positive patients, the cervix will be visualised during a follow up appointment for LBC or colposcopy. Decisions to perform a pelvic examination or visual inspection of the genital tract should be patient-centred, clearly clinically indicated and made collaboratively.

Resources
- ACPCC offers a free clinical advisory service and education on cervical screening for healthcare practitioners. Phone: (03) 9250 0309 Email: [email protected]
- ACPCCs Cervical Screening, HPV and Self-Collection Clinical Education Course is an in depth, self-paced online learning module, suitable for GPs and nurses, with CPD points available. To find out more and register for free click here.
- Further information on self-collection for practitioners is available here.
- More self-collection and cancer screening education is available on the ACPCC website here.
- Information resources for practitioners and patients are available here.
- Order the self-collection sampling instrument from VCS Pathology: (Flocked swab- Copan FLOQswab 552C, 552C.80 or 5E089N) here.
- If you are not currently a VCS Pathology practitioner, register here to receive self-collection test results.
- Cancer Council Victoria resources on self-collection (for consumers).
- You can easily check if the patient is overdue for screening by accessing the National Cancer Screening Register which has an online portal and integration with clinical systems.
- The National Cervical Screening Program website has information and up to date resources to support healthcare practitioners.
References
- Arbyn et al 2018. Detecting cervical precancer and reaching underscreened women by using HPV testing on self-samples: updated meta-analyses, BMJ 2018; 363:k4823, https://doi. org/10.1136/bmj.k4823
- Saville et al. Analytical performance of HPV assays on vaginal self-collected vs practitioner-collected cervical samples: the SCoPE study. J Clin Virol. 2020 Jun;127:104375. doi: 10.1016/j. jcv.2020.104375. Epub 2020 Apr 18. PMID: 32361328
- Creagh et al. (2021), Self-collection cervical screening in the renewed National Cervical Screening Program: a qualitative study. Med J Aust. https://doi.org/10.5694/mja2.51137
- Smith et al. (2021). Could HPV Testing on Self-collected Samples Be Routinely Used in an Organized Cervical Screening Program? A Modeled Analysis. Cancer Epidemiol Biomarkers Prev February 1 2021 (30) (2) 268-277; DOI:1158/1055-9965.EPI-20-0998
Media Enquiries
For more information about this campaign, please contact [email protected]
The Self-Collection Saves Lives campaign is supported by the Victorian Government.