12th Jan 2023: The Eastern Mediterranean Regional Office (EMRO) of the World Health Organisation (WHO) have developed a new cervical cancer elimination strategy with the guidance and support of the Australian Centre for the Prevention of Cervical Cancer (ACPCC) and the University of Melbourne.
In 2022, Australian cervical cancer elimination experts assisted EMRO with the development of a draft regional cervical cancer elimination strategy, drawing upon Australia’s effective cervical cancer screening program and its successful local elimination strategy.
The EMRO strategy has been developed in collaboration with 20 of its member states. With an estimated 320 million women in these states, if the strategy is implemented, these women and their families will benefit enormously either through vaccination, early detection, or treatment of cervical cancer – with nearly ALL cases of cervical cancer being preventable or treatable.
Executive Director of the ACPCC Professor Marion Saville said, “The barriers to eliminating this preventable disease are particularly acute in those countries where war and conflict is so significant, such as Yemen and Afghanistan, noting that the health sector in Afghanistan is primarily run by non-for-profit organizations which can now no longer employ women. HPV vaccines have been provided through schools in Afghanistan, meaning more than 50% of the target girls will be missed, as currently schooling is banned for girls over the 6th grade – this is a tragedy on a global scale”.
Prior to the announcement, only three of the 20 participating countries had existing national HPV vaccination programs (Libya, Kingdom of Saudi Arabia, United Arab Emirates), with the Saudi Arabian program having the widest range of people with a cervix targeted – covering those between the ages of 15 and 26.
The main barriers to achieving the global elimination targets that were identified across all member states were vaccine hesitancy – related to both stigma around HPV and safety concerns, and the cost of both HPV vaccines and HPV tests for screening.
Professor Saville noted the benefits of self-collect as an option, “With the stigma around HPV vaccination that still exists even in some high-income countries, and the barriers to accessing healthcare in low income and war-torn countries, the new self-collection tools are an incredibly important way in which we can still strive to eliminate this cancer. We estimated through work on EMRO’s elimination strategy that 60% of women in these countries would find self-collection of a HPV sample to be acceptable”.
For most countries, cancer treatment modalities were not widely available within the public sector. This is especially true for radiotherapy and palliative care, as only three countries each had wide access for the public.
In Australia, the National Strategy for the Elimination of Cervical Cancer aims to eliminate cervical cancer as a public health problem in Australia by 2035, making its experts suitable to draw upon for guidance and support in EMRO’s strategy development.
END
Additional Resources
In order to prepare the strategy, SitReps were compiled for 20 of the countries in the WHO Eastern Mediterranean Region, which provide a snapshot of these countries willingness and readiness to adopt the WHO’s Global Strategy to Accelerate the Elimination of Cervical Cancer as a public health problem. The sitreps are available and comprise of four sections: Country Overview; HPV Immunisation; Cervical Screening; and Cancer Treatment and Palliative Care.
Member states of the WHO Eastern Mediterranean Region

The Global Elimination 90-70-90 targets for 2030 are:
- 90% of girls are fully vaccinated by the age of 15 years
- 70% of women are screened with a high-performance test by age 35 years and again at 45 years
- 90% of women with pre-cancer are treated and 90% of women with invasive cancer are managed.
Summary of planned national cancer prevention and control strategies, HPV vaccination programmes and cervical screening programmes in the Eastern Mediterranean region.
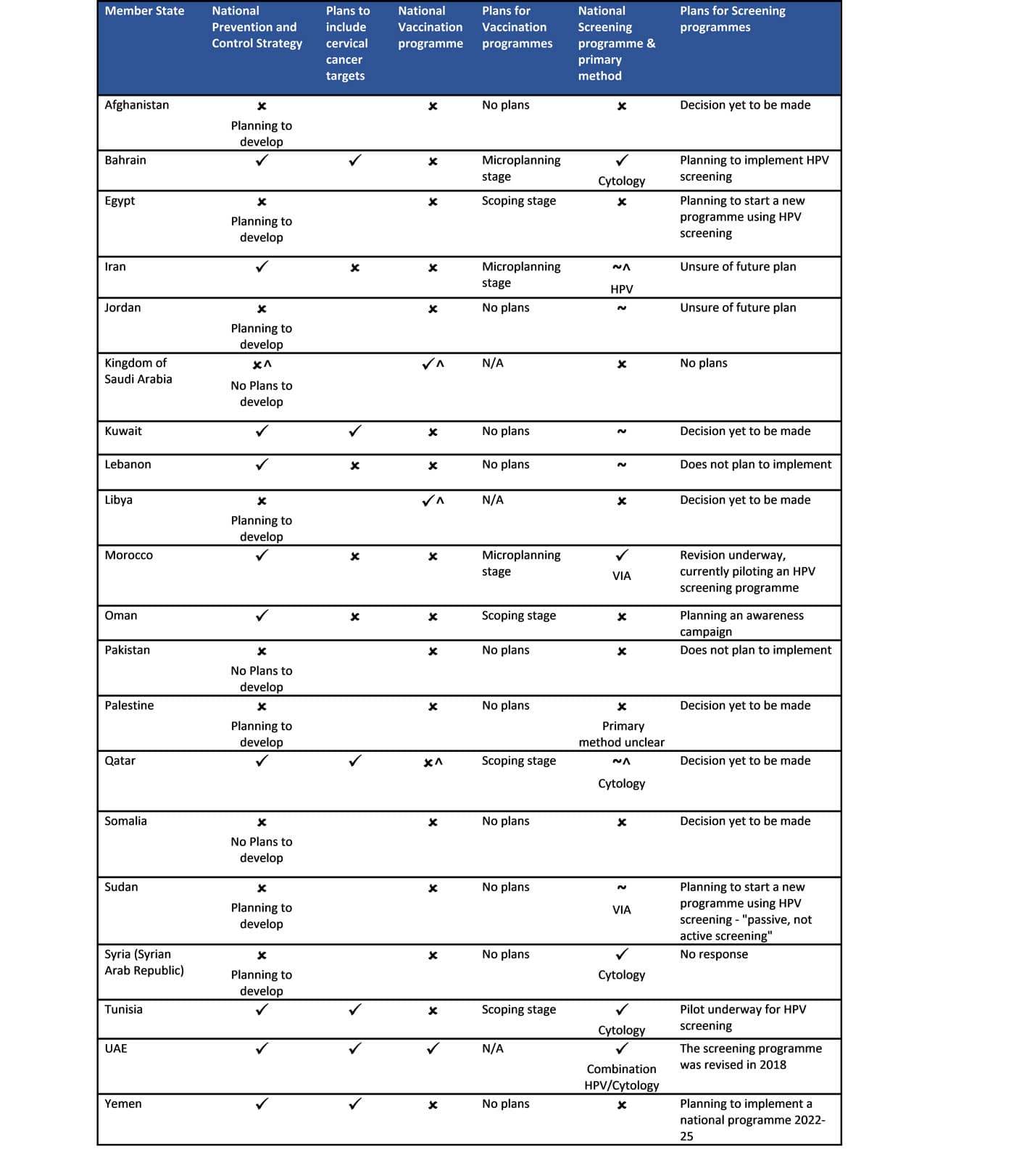
^Inconsistent with WHO country ✓ National programme ~ Subnational programme only
✗ No national or subnational programme. Note: No response from Djibouti or Iraq. *Consultation in August/Sept 22 indicated that the KSA does have a National Cancer Control Plan 2014-2025. **Microplanning stage – employing community action to inform and plan the development of a programme, utilising a bottom to top approach.
About the ACPCC
The Australian Centre for the Prevention of Cervical Cancer (ACPCC) is a not-for-profit organisation with over 50 years of expertise in cancer prevention and population health through laboratory and medical education services, establishing and operating cancer screening and vaccination registries, and conducting world-leading research and data analysis. ACPCC is working with Australian and international partners to achieve the World Health Organization’s goal of eliminating cervical cancer as a public health problem. Our team is committed to supporting the effective delivery of HPV vaccination and cervical screening programs, to ensure a cervical cancer free future for girls and women everywhere. www.acpcc.org.au
About the Centre for Health Policy, University of Melbourne
The Centre for Health Policy (CHP) strives to identify, critique, co-design, implement and evaluate policy options that protect the health of populations; to formulate, with partners, strategies that improve access, organisation, and delivery of health services or programs, particularly as they affect the most vulnerable; and to identify strategies for enhancing the safety, effectiveness and efficiency of health care systems in addressing the most pressing health and care challenges.